DOI: https://doi.org/10.34069/AI/2024.83.11.9
Volume 13 - Issue 83: 112-125 / November, 2024
How to Cite:
Klymenko, I., Reva, M., Lobanov, S., Lahodzinskyi, V., & Zaichykova, T. (2024). A scoping review of the effectiveness of cognitive-behavioral therapy in reducing ptsd symptoms in military personnel. Amazonia Investiga, 13(83), 112-125. https://doi.org/10.34069/AI/2024.83.11.9
A scoping review of the effectiveness of cognitive-behavioral therapy in reducing ptsd symptoms in military personnel
Revisión general de la eficacia de la terapia cognitivo-conductual para reducir los síntomas del TEPT en el personal militar
Received: October 20, 2024 Accepted: November 27, 2024
Written by:
Ivan Klymenko
https://orcid.org/0000-0003-3119-7494
Ph.D. Head of the Department, Associate Professor, Medical Psychology Department of Institute of Medical and Pharmaceutical Sciences, Department of Psychology of Educational and Scientific Institute of Psychology and Social Sciences, Interregional Academy of Personnel Management, Kyiv, Ukraine.
WoS Researcher ID: JGE-5112-2023 - Email: neffalimm@gmail.com
Maryna Reva
https://orcid.org/0000-0002-5478-8855
Ph.D. Associate Professor, Associate of the Professor Psychology Department, Faculty of Psychology and Social Work, Poltava V.G. Korolenko National Pedagogical University, Poltava, Ukraine.
WoS Researcher ID: INV-6075-2023 - Email: mreviera@ukr.net
Serhii Lobanov
https://orcid.org/0009-0002-6225-0200
M.D. PhD in Medicine, Associate Professor, Department of Pedagogy and Psychology, Faculty of Personnel Management, Kyiv National University of Economics, Kyiv, Ukraine. WoS Researcher ID: LIC-3932-2024 Email: sergej.lobanov.ua@gmail.com
Vitalii Lahodzinskyi
https://orcid.org/0000-0002-7081-9578
Ph.D. in History, Junior Researcher, Research Department of Applied Military and Sociological Studies, Scientific-Research Institute, Kyiv, Ukraine. WoS Researcher ID: KTI-3411-2024 - Email: logos2005@ukr.net
Tetiana Zaichykova
https://orcid.org/0000-0002-4194-4855
Ph.D. in Psychology, Associate Professor, Senior Trainer,
National Association of Gestalt Therapists of Ukraine, Kyiv Ukraine. WoS Researcher ID: LIY-9849-2024 Email: tatianazaichikova@gmail.com
Abstract
Posttraumatic stress disorder (PTSD) is a mental health condition that develops after experiencing or witnessing traumatic events. Cognitive behavioural therapy (CBT) is widely recognized as an effective evidence-based treatment for PTSD, particularly in military personnel. This study evaluates the efficacy of CBT for treating PTSD in this population. A systematic search of databases, including Web of Science, Google Scholar, Scopus, the Cochrane Library, and PubMed, identified 1807 studies using keywords such as "military," "veterans," "cognitive therapy," and "posttraumatic stress disorder." After screening titles and abstracts, 312 full-text articles were reviewed, with 51 publications meeting the inclusion criteria, which focused on RCTs, observational studies, meta-analyses, cohort studies, and case-control studies published since 2010. Non-peer-reviewed or unrelated articles were excluded. Findings reveal that CBT is effective in managing both acute and chronic PTSD, offering long-term and short-term benefits after various traumatic experiences. CBT is shown to be at least as effective as other psychological therapies, solidifying its role as a key treatment approach for PTSD in military personnel.
Keywords: cognitive therapy, posttraumatic stress disorder, mental disorder.
Resumen
El trastorno de estrés postraumático (TEPT) es un trastorno de salud mental que se desarrolla tras experimentar o presenciar acontecimientos traumáticos. La terapia cognitivo-conductual (TCC) está ampliamente reconocida como un tratamiento eficaz basado en la evidencia para el TEPT, particularmente en el personal militar. Este estudio evalúa la eficacia de la TCC para tratar el TEPT en esta población. Una búsqueda sistemática en bases de datos, incluyendo Web of Science, Google Scholar, Scopus, la Biblioteca Cochrane y PubMed, identificó 1807 estudios utilizando palabras clave como «militar», «veteranos», «terapia cognitiva» y «trastorno de estrés postraumático». Después de examinar los títulos y resúmenes, se revisaron 312 artículos de texto completo, con 51 publicaciones que cumplían los criterios de inclusión, que se centraron en ECA, estudios observacionales, metanálisis, estudios de cohortes y estudios de casos y controles publicados desde 2010. Se excluyeron los artículos no revisados por pares o no relacionados. Los hallazgos revelan que la TCC es eficaz en el manejo del TEPT agudo y crónico, ofreciendo beneficios a largo y corto plazo después de varias experiencias traumáticas. La TCC ha demostrado ser al menos tan eficaz como otras terapias psicológicas, consolidando su papel como un enfoque de tratamiento clave para el TEPT en el personal militar.
Palabras clave: terapia cognitiva, trastorno de estrés postraumático, trastorno mental.
Introduction
Background
PTSD is a chronic impairing condition that develops following exposure to accidents that cause trauma. This illness can disrupt family and individual functioning, creating substantial financial, medical, and social problems. Veterans and active duty personnel are more likely to experience trauma and develop mental health issues. PTSD affects an estimated 21–41% of veterans who have returned from recent conflicts, while 7–15% experience syndromal depression (Song et al., 2020). Nightmares and Insomnia are common in people with PTSD and may be signs of the disorder itself or partially separate conditions (Krasnodemska et al., 2023). The present treatments for PTSD do not work well for sleep disruptions, and the results of PTSD treatment are worse for patients who also experience sleeplessness and nightmares. Furthermore, there is a risk of depression, anxiety, substance misuse, and suicide associated with sleeplessness and nightmares (Peterson et al., 2020).
Three subgroups exist within the various pharmacological and psychological types that currently address PTSD prevention: primary type, which takes place prior to the situations that cause trauma and involves preventing the event itself; secondary type, which occurs in the interim between the traumatic incident and the onset of PTSD; and tertiary type, which occurs after the PTSD symptoms start to show (Baig et al., 2021). Pharmacological therapies have shown encouraging outcomes in reducing the intensity of PTSD symptoms, while their total impact is small. A recent thorough review and meta-analysis of 21 studies carried out in 2021 found that selective serotonin reuptake inhibitors (SSRIs) such as sertraline, fluoxetine, and paroxetine, as well as the serotonin-norepinephrine reuptake inhibitor (SNRI) venlafaxine and the atypical antipsychotic quetiapine, were effective as separate therapies for PTSD (Fredman et al., 2020).
PTSD in adolescents and children is commonly treated in psychotherapy with cognitive behavioral therapy (Malarkey et al., 2024). By doing away with avoidant and safety-seeking behaviors that prevent people from self-correcting incorrect ideas, cognitive behavioral therapy helps people control their stress levels, which in turn lowers the risk of stress-related diseases and enhances mental health. A sort of psychotherapy called cognitive behavior therapy helps patients identify and change unhelpful or disturbing thought habits that have a negative influence on their behavior and emotions (Paiva et al., 2024).
Problem statement
Many veterans of the military forces suffer from post-traumatic stress disorder (PTSD). Changes in thoughts and emotions, discomfort in the body or mind, trouble sleeping, and unsettling thoughts, dreams, or feelings linked to the incidents are some of the symptoms. The quality of life for these individuals and their families is impacted by each of these symptoms.
Research focus
What researchers discover regarding the role of cognitive-behavioral therapy in the management of PTSD in military personnel, and what they might know or learn, has an impact on society at large, clinical practice, and research. Our review focused on these implications to determine the best option for the management of PTSD in military personnel.
Research questions
Research objectives
In this review, we aim to investigate the role of cognitive-behavioral therapy in the management of post-traumatic stress disorder in military personnel.
Literature review
PTSD is a mental health illness that occurs after witnessing or going through a stressful event. Combat exposure, natural catastrophes, sexual or physical assault, accidents, and other potentially life-threatening scenarios are all common PTSD triggers. PTSD symptoms might involve nightmares, flashbacks, hyperarousal, intrusive thoughts, avoidance of traumatic memories, and a lack of emotion (Tanev et al., 2020). It can have a substantial impact on a person's everyday life, relationships, and general health. PTSD is a curable disorder, and successful interventions such as trauma-focused psychotherapies (TFP) and pharmaceutical medications can assist patients in coping with and recovering from the impacts of trauma (Demchenko, Zahariichuk, Dergach, Porodko, & Pryzvanska, 2022). Early recognition and adequate assistance can make a significant difference in the course of recovery (Sloan et al., 2020).
Prevalence and importance
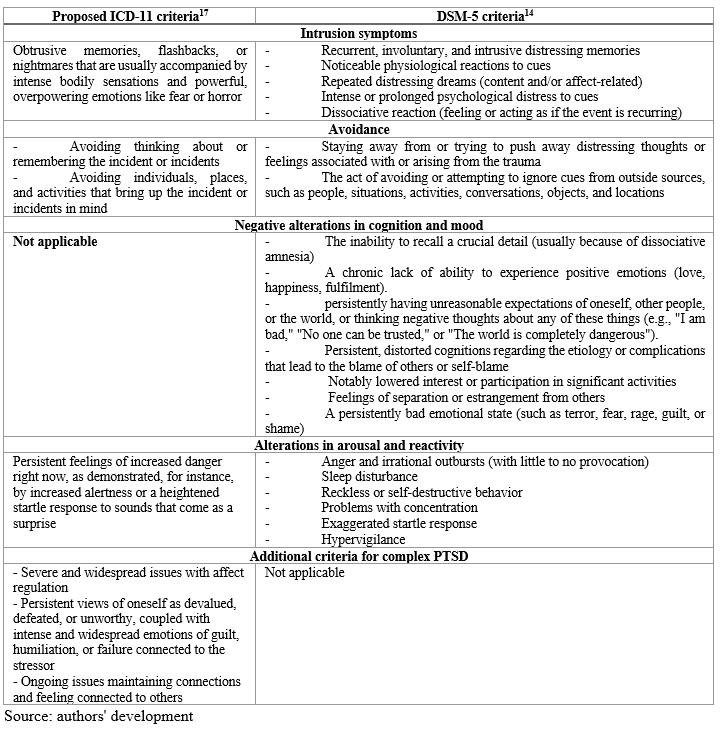
PTSD is often associated with poor personal outcomes, including physical health problems and co-occurring illnesses such as substance dependence. Data from the DSM-5 indicate that more than 80% of individuals with PTSD also experience one or more comorbid conditions. For instance, 48% of those with PTSD also have a concurrent mild traumatic brain injury. Additionally, there are significant links between PTSD and cognitive decline (Ma’ruf et al., 2024). Veterans and active military personnel exhibit a documented incidence rate of PTSD ranging from 5.4% to 16.8%, which is more than double that of the general population (Malarkey et al., 2024). Variations in these estimates depend on the patient population under investigation, the nature of traumatic incidents, and the methodology used for evaluation (Huda, 2023). The recent surge in international terrorism and armed conflict highlights the severe impact of PTSD. While this condition can affect individuals of any age, the majority of recent research focuses on returning veterans, making the military community a significant contributor to the body of knowledge on PTSD. Despite these advances, there remain notable gaps in research. Limited attention has been given to the effects of PTSD on children, leaving an important area of study underexplored (Fry et al., 2024).
Course of PTSD
For a long time, it was thought that PTSD developed linearly following trauma exposure, with the majority of patients seeing a remission of symptoms during the months that followed. Numerous studies showed that PTSD rates decreased six months after trauma compared to rates in the weeks following the incident provided evidence in favor of this theory (Gorinov & Mereniuk, 2022). Delay-onset PTSD, which the Diagnostic and Statistical Manual of Mental Disorders (DSM) has historically described as the onset of PTSD that appears at least half a year after the distressing event, was the exception to this pattern (Malaktaris et al., 2022).
Recent data has cast doubt on the idea that PTSD progresses in a straight line, suggesting instead that a person's status is not static and that the disorder's intensity varies over time, sometimes getting worse and sometimes getting better. The trajectories of PTSD have been mapped using latent growth mixture modeling in recent studies. These maps reliably show that there are four classes: delayed reaction, which initially exhibits low levels of symptoms but eventually increases them, recovery, which shows a consistent reduction in PTSD symptoms, and chronic distress, which shows a constant increase in symptoms, a resilient class which consistently has few symptoms of PTSD (Bryan et al., 2022). Network analysis, which takes into account the degree of links between symptoms, also provides evidence for the progressive nature of the PTSD illness (Miloradova, 2023). During the initial acute phase following trauma, symptoms of PTSD seem to be less closely associated with established factors, such as active avoidance and re-experiencing, but over time they become more tightly tied (LoSavio et al., 2023).
Symptoms of PTSD
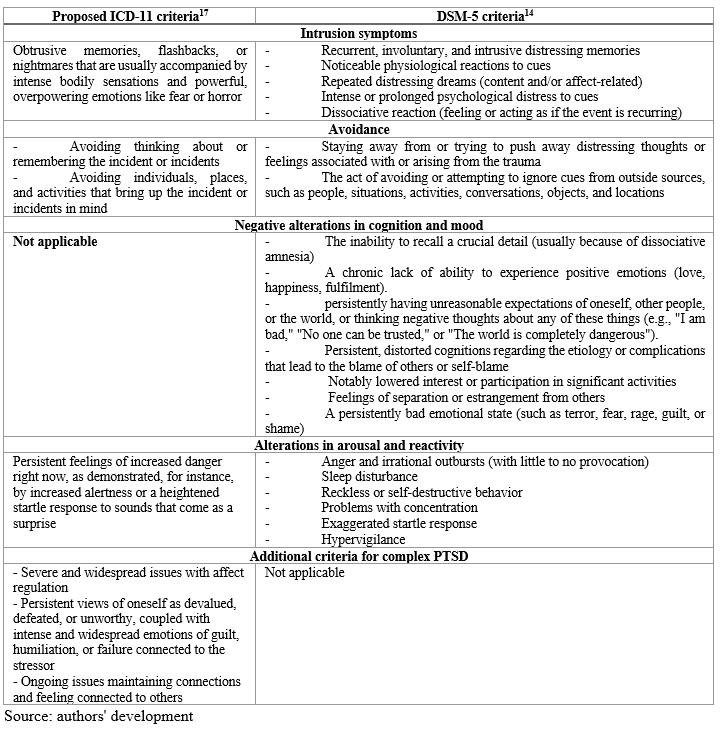
Constantly unpleasant memories, avoiding triggers associated with the trauma, unfavorable changes in mood and thought patterns, and hyperarousal are some of the symptoms (table 1). Based on DSM-5 criteria, a person can be diagnosed if their ability to operate normally has been markedly hindered for a month. It is not uncommon for symptoms to manifest years later, even in cases where the consequences are severe (Skopp, Kaplan, Todd, Drell, & Pratt, 2023).
Table 1.
Symptoms of PTSD
Symptom Overlap and Comorbidity in PTSD
According to the DSM-5, PTSD shares many physiological symptoms with substance use disorders, major depressive disorder (MDD), and other anxiety disorders, as well as other mental health conditions.
Epidemiological data from the National Comorbidity Survey conducted in 1995 reveal that at least three additional mental illnesses were present in 59% of males and 44% of females with PTSD. A long-term epidemiological survey indicates that approximately 91% of individuals with PTSD also meet the criteria for other psychiatric disorders.
The significant symptom overlap makes it challenging to differentiate PTSD from complex mental disorders in certain cases, particularly when trauma histories are unclear (Pokharel et al., 2024).
A substantial proportion of individuals with PTSD also receive a diagnosis of major depressive disorder (MDD) despite these being distinct conditions (Schnurr et al., 2022). Depression is especially likely to co-occur with PTSD following traumatic events.
PTSD symptoms that are nonspecific include the NACM and hyperarousal clusters, which overlap significantly with symptoms of MDD. Common symptoms of both PTSD and MDD include difficulties with concentration, sleep disturbances, social withdrawal, avoidance behaviours, reduced cognitive functioning, and a lack of interest or pleasure in positive activities (Zaitsev, 2023).
Mood-related symptoms associated with both PTSD and MDD are typically long-lasting, often persisting for several months. A study on DSM-5 criteria for PTSD and depression found that higher levels of somatic and affective depression correlated with increased NACM symptom severity, which, in turn, was linked to greater PTSD severity (Peterson et al., 2022).
PTSD and Military
It is often recognized that both veterans and active military people frequently endure severe stress and go through a variety of traumatic, potentially fatal experiences. They thus have an especially high chance of experiencing PTSD, which may be considered PTSD connected to the military. In operational infantry battalions, the frequency of PTSD connected to military service following deployment to Afghanistan or Iraq was demonstrated to be 13.2%. According to different databases, 11% of soldiers still experienced symptoms of PTSD forty years later after the war in Vietnam (Sloan et al., 2022). Furthermore, an analysis of the frequency of PTSD in veterans found that up to 23% of them had the disorder. It was shown that PTSD and alcohol abuse were the most prevalent mental illnesses that military personnel assigned to conflict zones reported having. It was shown that alcohol abuse and PTSD were the most prevalent mental illnesses mentioned by military members sent to war zones (Perez Garcia et al., 2021).
However, it has been discovered that alcohol abuse is far more common than previously thought to exist in people and may prolong the PTSD course. It is also mentioned that service personnel who suffer from mental illnesses, particularly PTSD, may feel stigmatized strongly. This is because they may be afraid of what their peers and military leadership would think of them, which prevents them from getting the competent medical care they need. Thirteen Since PTSD related to military service negatively affects the army's combat effectiveness, appropriate steps should be taken to address this problem (Macdonald et al., 2022). Numerous pharmaceutical and psychosocial therapies are now being used to treat PTSD. Numerous studies have been conducted on the effectiveness of psychotherapies, which are often classified as "trauma-focused" or "non-trauma-focused." (Christ et al., 2022).
The guidelines state that the treatments with the most evidence from clinical trials are prolonged exposure, cognitive behavior therapy, and eye movement desensitization and reprocessing. Evidence-based treatment alternatives for non-trauma-focused psychotherapies include present-centered therapy, interpersonal psychotherapy, and stress inoculation training. Treatment for PTSD also frequently involves the use of pharmacotherapies (Andersen et al., 2021).
Table 2.
Prevalence of PTSD in military personnel and veterans
Cognitive Therapy in PTSD Treatment
Overview of Cognitive Behavior Therapy Cognitive behavior therapy (CBT) is structured, didactic, and goal-oriented. This practical, interactive approach involves the patient and therapist working together to modify thought and behavior patterns to enhance the patient's quality of life and overall mood. Therapeutic procedures are tailored to the patient's diagnosis and challenges, with most cognitive-behavioral psychotherapists customizing care to meet each client's specific needs (LoSavio et al., 2021).
Evidence-Based Therapies for PTSD There are numerous evidence-based therapies for PTSD, with CBT being the most researched. Originally designed for rape survivors, CBT has been used for various trauma types and demographics, including active-duty military personnel and veterans. Numerous RCTs have confirmed CBT's effectiveness in veteran populations. Recent RCTs have shown CBT to be effective in treating PTSD in military personnel (Alavi et al., 2021).
Effectiveness in Military Populations Although CBT has generally been beneficial for military samples, some data indicate less stable outcomes. The effect sizes in two RCTs with active-duty participants were medium-to-large but smaller than those typically observed in other samples, with less improvement in depression symptoms. A meta-analysis indicated that PTSD treatments were less effective for combat-related PTSD compared to other trauma types (Resick et al., 2021).
Methodology
General Background
The trauma exposures, comorbidity and mental disease rates, and treatment response of military and veteran groups are distinct. The extent to which cognitive behavioral therapy may be suitable for veterans and military people is yet unknown, despite reviews indicating that cognitive behavior therapy can be helpful in treating mental health issues. Although most reviews concur that cognitive behavioural therapy has potential benefits for treating mental health issues, authors have identified a number of constraints that could impact assessments of cognitive behaviour therapy 's efficacy and applicability.
Inclusion Criteria:
Exclusion criterio
Information Sources
Data Collection
Justification for Choice of Databases
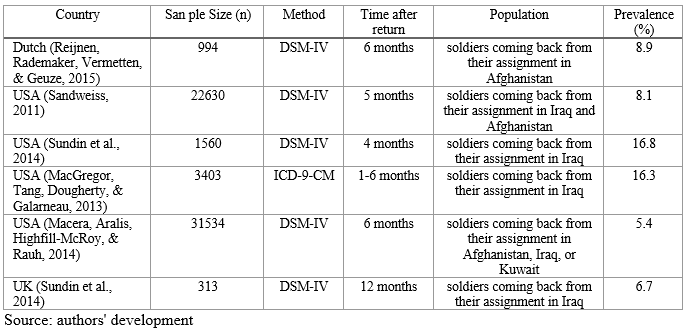
A comprehensive literature search was performed using multiple online databases, including Web of Science, Google Scholar, Scopus, Cochrane Library, and PubMed. These databases were selected due to their relevance and reliability in providing high-quality academic sources. Web of Science offered extensive coverage of scientific research across various disciplines, enabling access to various peer-reviewed articles. Google Scholar facilitated access to diverse academic literature, including theses, books, and conference papers, ensuring that relevant studies were not overlooked. As one of the largest abstract and citation databases, Scopus provided thorough coverage of scientific, technical, and medical research, which was critical for this analysis. The Cochrane Library, recognized for its systematic reviews and meta-analyses of clinical trials, contributed high-quality, evidence-based studies. PubMed offered an extensive repository of biomedical and life sciences literature, which was indispensable for identifying studies focusing on PTSD and cognitive therapy.
The search was conducted using specific keywords, including “military,” “veterans,” “cognitive therapy,” “mental disorder,” and “posttraumatic stress disorder.” This approach ensured that a comprehensive range of academic articles relevant to the research topic was included in the analysis.
Data collection
Three steps were engaged in the review of the involved studies. The first step was importing the search strategy's findings from electronic databases into a sheet of Microsoft Excel using EndNote software. The articles' titles and abstracts that were entered into the sheet of Excel were filtered in the second stage. The evaluation of the relevant citations from Stage 2's complete text came next. We also double-checked the research references to make sure no ones were overlooked.
Statistical analysis
We carried out a qualitative analysis of the earlier research findings. Since our study is a systematic review, we were unable to do a quantitative analysis. In order to draw conclusions, it is necessary to identify and compare more than two studies that provide data on the outcomes that will be examined in the quantitative analysis. In our research, we tried a quantitative analysis, but we were unable to locate particular findings that were pertinent to our topic or publications that offered comparable data. We carried out a qualitative examination of articles pertinent to our topic, presented their findings, and compared them in order to obtain solid proof as well as up-to-date results and conclusions.
Results
The search approach yielded 1807 articles. A review of these articles was conducted to identify those relevant to the research topic. Following the screening of titles and abstracts, 312 articles underwent full-text review. For the purposes of data compilation and analysis, as well as for writing on the subject, 51 publications were ultimately included (Figure 1,2).
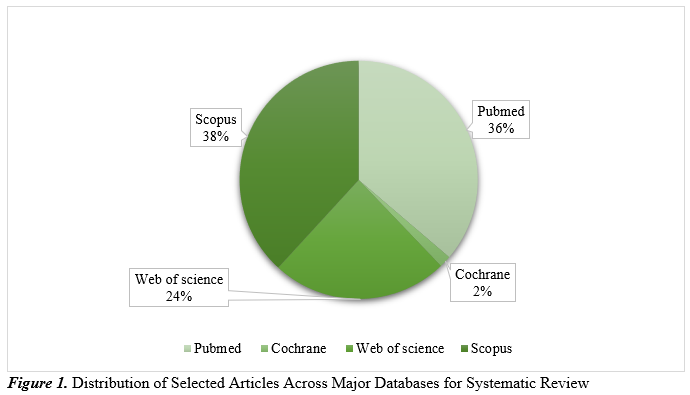
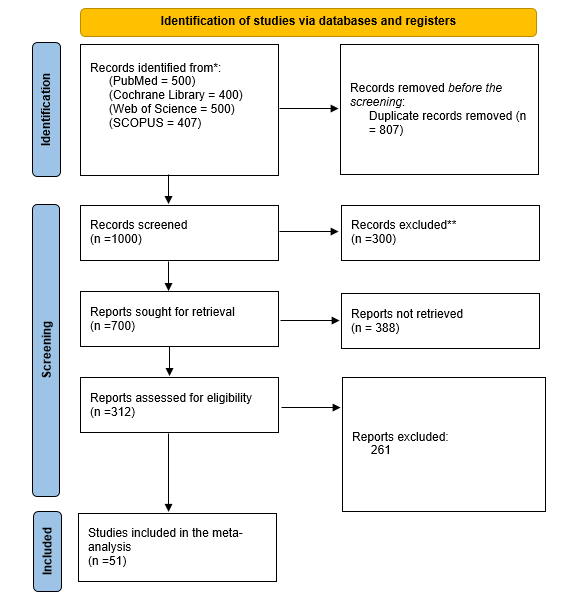
Figure 2. PRISMA flow chart of our literature search.
Source: authors' development
Heller et al. involved a total of 123 patients. All participants got the group-delivered cognitive behavior therapy intervention for the first 12 weeks of treatment (Phase 1), and after that, they were randomly assigned to attend 12 weekly 60-minute individual cognitive behavior therapy sessions (Phase 2). The end of cognitive behavior therapy was found to have a minor positive impact on PTSD and depressive symptoms, which persisted a year later after receiving Phase 2 individual treatment. Participants in the trauma-focused Phase 2 therapy demonstrated similar levels of symptom reduction and maintenance of treatment improvements as compared to those in the non-trauma-focused Phase 2 treatment. For veterans with a history of trauma, depression, and SUD, cognitive behavior therapy seems to be beneficial overall (Haller et al., 2016).
The research now shows compelling evidence that cognitive behavior therapy is a safe and effective treatment for both acute and chronic PTSD following a range of traumatic events in children, adults, and adolescents. Up to 50% of PTSD patients do not respond to cognitive behavior therapy, which could be caused by comorbidity and the study sample's demographics. In a variety of cultural situations, cognitive behavior therapy has been validated and successfully used by community therapists who have undergone brief training in both group and individual settings. PTSD has been successfully treated with web-based cognitive behavioral therapy. There is little data to offer firm recommendations, but some studies have shown that cognitive behavior therapy can serve as a preventive measure. The alteration in maladaptive cognitive functioning linked to PTSD has mostly acted as a mediator for the effects of cognitive behavior therapy. Numerous studies also document alterations in electroencephalography, functional neuroimaging, and physiology that are correlated with cognitive behavior therapy response (Kar, 2011).
Four equal interventional cohorts were randomly assigned to the participants in a prior study: (cohort a) problem-solving therapy; (cohort b) exposure therapy; (cohort c) combined therapy (exposure therapy with problem-solving); and (cohort d) a control cohort. Using the GSI and SF36 scores, they discovered that the mean SF36 scores for the participants at baseline were 36.4±3.2 for cohort (a), 41.18±2.4 for cohort (b), 35.53±3.3 for cohort (c), and 45.9±4.6 for cohort (d). The mean SF36 scores considerably improved after the study intervention. After a follow-up period, the mean SF36 scores showed an identical significant improvement. At baseline, the mean GSI of the patients in cohorts (a), (b), (c), and (d) was 1.78±0.3, 1.62±0.3, and 1.85±0.2, respectively. The mean GSI significantly improved as a result of the research intervention. After a period of observation, the average GSI demonstrated an equally noteworthy improvement (Ahmadizadeh et al., 2013).
In order to assess the relative effectiveness of prolonged exposure (PE) and cognitive behavior therapy in enhancing intimacy functioning in active service military personnel with PTSD or veterans and their intimate partners, a randomized controlled trial was conducted. There was a general consistency for relationship outcomes, where PE did not demonstrate any improvement while CBCT produced notable improvements. Relationship satisfaction between service members and veterans, relationship satisfaction between partners, and relationship problems as rated by service members and veterans all showed this pattern. In terms of PTSD outcomes, both conditions showed substantial improvements in both self-reported and clinician-rated PTSD symptoms. In the cognitive behavior therapy cohort, partner-reported PTSD symptoms dramatically got better but not in the PE cohort (Monson et al., 2024).
Discussion
Studies on the treatment of patients with PTSD have focused on both psychotherapy and medication. Several studies have used cognitive behaviour therapy to treat PTSD, with the finding that it is the first-line treatment for PTSD connected to conflict, particularly in chronic patients. Cognitive behaviour therapy has shown promise as a treatment for PTSD sufferers and has the potential to reduce symptoms more quickly. According to patients with PTSD, they showed the best outcomes from cognitive therapy within the first two months of their treatment. PTSD may negatively impact QOL in both non-veterans and veterans, and a recent meta-analysis on QOL in individuals with anxiety disorders discovered that, among other factors, PTSD was the primary source of QOL impairment in these patients (Peterson et al., 2020).
The results of the cognitive behavior therapy treatments were consistent with previous meta-analyses of cognitive behavior therapy sessions on depression (d = 0.41) and PTSD (d = -0.60) carried out with non-military samples, and the benefits were strong across a variety of primary and secondary research outcomes (Andersson et al., 2014). This demonstrates how effective cognitive behavior therapy is. Furthermore, the size of our results (g = 0.54) was comparable to other research on cognitive behavior therapy for depression (g = 0.71) and PTSD in general society (g = 0.72) (Sijbrandij et al., 2016). The relative similarity of these results, despite their significantly lower sample size, confirms the validity of cognitive behavior therapy in general and their adaptability to a variety of delivery methods, such as phone, app, and internet-based delivery. Cognitive behavior therapies were found to be differently beneficial based on a number of parameters in addition to the gathered effects (Taylor et al., 2017). Enhancements in symptoms were more pronounced for participants getting additional therapies, such as medication and adjuvant therapies, in addition to cognitive behavior therapy, than for those not receiving additional therapies (Liu et al., 2023).
It's significant in and of itself that there may be a correlation between treatment preference and an interest in how relationships function. Recognising that PTSD sufferers are a diverse group with a range of motivations for seeking treatment as well as preferred treatments is crucial (Meis et al., 2019). Previous research shows that having close relationships is a major factor in encouraging people to seek treatment for PTSD and that the functioning of couples' and families' relationships is linked to the chance of completing trauma-focused PTSD therapy and the results obtained. Furthermore, it is commonly known that patient preferences have a significant role in therapy participation and outcomes for a range of illnesses. To increase the chance that PTSD sufferers and their loved ones will participate in and benefit from treatment, it is crucial to provide a variety of efficient treatments (Windle et al., 2020).
When compared to male and military subgroups, the improved PTSD symptoms in civilian and female populations at follow-up match earlier findings at short- and medium-term follow-up. Notably, the results of treatment for PTSD did not vary with respect to the period of follow-up, suggesting that improvements in symptoms continued for more than a year following treatment. There are currently few trials with extended follow-up periods, and further research is needed to prove therapy benefits beyond a year after treatment (Kline et al., 2018).
The results of this study are encouraging because, in veteran and service member populations, PTSD can be challenging to treat. Veterans showed improvements in their functional disability, comorbid symptoms of anxiety and sadness, and PTSD. In addition, the individuals expressed a high degree of satisfaction with the treatment. The study contributes to the increasing body of research demonstrating that trauma-focused group therapy had smaller impact sizes than trauma-focused individual therapy. The present study adds credence to the increasing body of research, especially pertaining to the veteran and service-member populations, that has not discovered any appreciable variations between conditions for treatments that are trauma-focused and those that are not (Hoge & Chard, 2018; Steenkamp et al., 2015).
After discovering about the treatment at Session 1, active duty military people generally felt that it was credible and had high expectations for it. When evaluated one week after the last session, these favorable expectations continued throughout treatment, which is significant because behavioral treatments rely on patients' willingness to participate in the treatment's activities (Pruiksma et al., 2018). The study found that active duty service members might do well in activities involving nightmare exposure and rewriting. Comparing the rates of treatment initiation to civilian studies, they were somewhat higher. Given how mobile active duty service members are and how frequently they move between duty posts, this is especially noteworthy. Among active-duty military soldiers, cognitive behavior therapy significantly reduced the number of PTSD measures. Participants believed that cognitive behavior therapy was both practical and credible (Pruiksma et al., 2020).
Limitations
Despite the comprehensive search and selection process, several limitations were identified in this scoping review. The heterogeneity of study designs posed significant challenges. The included studies employed diverse methodologies, such as randomized controlled trials, cohort studies, and observational studies, which prevented the feasibility of a meta-analysis. Variations in study designs and outcome measures further limited the ability to conduct quantitative synthesis, reducing the potential to draw robust statistical conclusions across studies.
Language and date restrictions also presented constraints. The review included only studies published in English since 2010, potentially excluding relevant research published in other languages or earlier studies that could have provided valuable context and additional insights.
Another limitation was the narrow focus on specific populations. Most of the studies examined veterans and active-duty military personnel, with minimal attention to other groups, such as children or individuals with non-combat-related PTSD. This limited focus reduces the generalizability of the findings to broader populations affected by PTSD.
Conclusions
This review highlights that cognitive behaviour therapy (CBT) is an effective treatment for both chronic and acute post-traumatic stress disorder (PTSD), with significant short- and long-term benefits. The findings indicate that CBT is at least as effective as other psychological therapies, consistently improving quality of life during treatment. Notably, the most substantial symptomatic improvements are observed within the first three months, with 60% of patients experiencing symptom relief.
These findings have important implications for both theory and practice. They underscore the importance of early intervention in PTSD treatment and suggest that CBT should be considered a first-line therapeutic option for military personnel and other populations affected by trauma. Additionally, the results contribute to the growing body of evidence supporting CBT’s role in enhancing the quality of life for PTSD patients.
For future research, focusing on identifying predictive characteristics and physiological markers could help develop preventive strategies, reducing the incidence of PTSD and its broader societal impact. This study’s contribution lies in consolidating the evidence for CBT’s effectiveness in diverse trauma scenarios and offering new avenues for targeted interventions.
Acknowledgments: None
Ethical statement: Not applicable.
Funding: None
Conflict of interest: None
Bibliographic references
Ahmadizadeh, M., Ahmadi, K., Anisi, J., & Ahmadi, A. B. (2013). Assessment of Cognitive Behavioral Therapy on Quality of Life of Patients with Chronic War-related Post-traumatic Stress Disorder. Indian Journal of Psychological Medicine, 35(4), 341–345. https://doi.org/10.4103/0253-7176.122222
Alavi, N., Stephenson, C., Omrani, M., Gerritsen, C., Martin, M. S., Knyahnytskyi, A., … & Groll, D. (2021). Delivering an Online Cognitive Behavioral Therapy Program to Address Mental Health Challenges Faced by Correctional Workers and Other Public Safety Personnel: Protocol for a Mixed Methods Study. JMIR Research Protocols, 10(7), e30845. https://doi.org/10.2196/30845
Andersen, M. R., Clausen, A., Sternhagen Nielsen, A. B., & Hjort Svendsen, A. L. (2021). Experiences with basic body awareness therapy as an add-on to cognitive behavioral therapy among Danish military veterans with PTSD: An interview study. Journal of Bodywork and Movement Therapies, 27, 550–559. https://doi.org/10.1016/j.jbmt.2021.03.023
Andersson, G., Cuijpers, P., Carlbring, P., Riper, H., & Hedman, E. (2014). Guided Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry, 13(3), 288–295. https://doi.org/10.1002/wps.20151
Baig, M. R., Ouyang, S., Mata-Galán, E., Dawes, M. A., & Roache, J. D. (2021). A Comparison of Cognitive Processing Therapy and Seeking Safety for the Treatment of Posttraumatic Stress Disorder in Veterans. Psychiatric Quarterly, 92(2), 735–750. https://doi.org/10.1007/s11126-020-09850-2
Bryan, C. J., Russell, H. A., Bryan, A. O., Rozek, D. C., Leifker, F. R., Rugo, K. F., … & Asnaani, A. (2022). Impact of Treatment Setting and Format on Symptom Severity Following Cognitive Processing Therapy for Posttraumatic Stress Disorder. Behavior Therapy, 53(4), 673–685. https://doi.org/10.1016/j.beth.2022.01.014
Christ, N. M., Blain, R. C., Pukay-Martin, N. D., Petri, J. M., & Chard, K. M. (2022). Comparing Veterans with Posttraumatic Stress Disorder Related to Military Sexual Trauma or Other Trauma Types: Baseline Characteristics and Residential Cognitive Processing Therapy Outcomes. Journal of Interpersonal Violence, 37(21–22), NP20701–NP20723. https://doi.org/10.1177/08862605211055082
Demchenko, I., Zahariichuk, O., Dergach, M., Porodko, M., & Pryzvanska, R. (2022). The psychological and pedagogical aspect of the life quality of citizens with disabilities. Amazonia Investiga, 11(54), 339–348. https://doi.org/10.34069/AI/2022.54.06.32
Gorinov, P., & Mereniuk, K. (2022). Military law in Ukraine: future prospects for development. Futurity Economics&Law, 2(3), 18–27. https://doi.org/10.57125/FEL.2022.09.25.03
Fredman, S. J., Macdonald, A., Monson, C. M., Dondanville, K. A., Blount, T. H., Hall-Clark, B. N., … & Peterson, A. L. (2020). Intensive, Multi-Couple Group Therapy for PTSD: A Nonrandomized Pilot Study With Military and Veteran Dyads. Behavior Therapy, 51(5), 700–714. https://doi.org/10.1016/j.beth.2019.10.003
Fry, K. M., Bennett, D. C., Roberge, E. M., McClain, C. M., Rugo-Cook, K., Brewczynski, J., & Pryor, C. (2024). The effects of Religiosity, Spirituality, and sense of purpose on posttraumatic stress disorder treatment outcomes among Veterans. Journal of Psychiatric Research, 176, 276–281. https://doi.org/10.1016/j.jpsychires.2024.05.054
Haller, M., Norman, S. B., Cummins, K., Trim, R. S., Xu, X., Cui, R., … & Tate, S. R. (2016). Integrated Cognitive Behavioral Therapy Versus Cognitive Processing Therapy for Adults With Depression, Substance Use Disorder, and Trauma. Journal of Substance Abuse Treatment, 62, 38–48. https://doi.org/10.1016/j.jsat.2015.11.005
Hoge, C. W., & Chard, K. M. (2018). A Window Into the Evolution of Trauma-Focused Psychotherapies for Posttraumatic Stress Disorder. JAMA, 319(4), 343. https://doi.org/10.1001/jama.2017.21880
Huda, O. (2023). Use of the Moodle Platform in Higher Education Institutions During Training Masters: Experience Under Martial Law. E-Learning Innovations Journal, 1(2), 4–20. https://doi.org/10.57125/ELIJ.2023.06.25.01
Kar, N. (2011). Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: a review. Neuropsychiatric Disease and Treatment, 167. https://doi.org/10.2147/NDT.S10389
Kline, A. C., Cooper, A. A., Rytwinksi, N. K., & Feeny, N. C. (2018). Long-term efficacy of psychotherapy for posttraumatic stress disorder: A meta-analysis of randomized controlled trials. Clinical Psychology Review, 59, 30–40. https://doi.org/10.1016/j.cpr.2017.10.009
Krasnodemska, I., Savitskaya, M., Berezan, V., Tovstukha, O., & Rodchenko, L. (2023). Psychological consequences of warfare for combatants: ways of social reintegration and support in Ukraine. Amazonia Investiga, 12(70), 78–87. https://doi.org/10.34069/AI/2023.70.10.7
Liu, J. J., Ein, N., Forchuk, C., Wanklyn, S. G., Ragu, S., Saroya, S., … Richardson, J. D. (2023). A meta-analysis of internet-based cognitive behavioral therapy for military and veteran populations. BMC Psychiatry, 23(1), 223. https://doi.org/10.1186/s12888-023-04668-1
LoSavio, S. T., Hale, W. J., Moring, J. C., Blankenship, A. E., Dondanville, K. A., Wachen, J. S., … & Resick, P. A. (2021). Efficacy of individual and group cognitive processing therapy for military personnel with and without child abuse histories. Journal of Consulting and Clinical Psychology, 89(5), 476–482. https://doi.org/10.1037/ccp0000641
LoSavio, S. T., Straud, C. L., Dondanville, K. A., Fridling, N. R., Wachen, J. S., McMahon, C. J., … Resick, P. A. (2023). Treatment responder status and time to response as a function of hazardous drinking among active-duty military receiving variable-length cognitive processing therapy for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 15(3), 386–393. https://doi.org/10.1037/tra0001268
Ma’ruf, M. R., Anggeria, E., Siregar, R. F., Sinaga, E. S., Aminah, Rahmi, I. M., … & Kaban, F. B. (2024). Application of Swedish Massage Therapy for Lower Extremities to Alleviate Muscle Cramps in Chronic Kidney Disease Patients. Futurity Medicine, 3(4). https://doi.org/10.57125/FEM.2024.12.30.01
Macdonald, A., Fredman, S. J., Taylor, D. J., Pruiksma, K. E., Blount, T. H., Hall‐Clark, B. N., … Peterson, A. L. (2022). Secondary individual outcomes following multicouple group therapy for posttraumatic stress disorder: An uncontrolled pilot study with military dyads. Journal of Traumatic Stress, 35(1), 321–329. https://doi.org/10.1002/jts.22729
Macera, C. A., Aralis, H. J., Highfill-McRoy, R., & Rauh, M. J. (2014). Posttraumatic Stress Disorder After Combat Zone Deployment Among Navy and Marine Corps Men and Women. Journal of Women’s Health, 23(6), 499–505. https://doi.org/10.1089/jwh.2013.4302
MacGregor, A. J., Tang, J. J., Dougherty, A. L., & Galarneau, M. R. (2013). Deployment-related injury and posttraumatic stress disorder in US military personnel. Injury, 44(11), 1458–1464. https://doi.org/10.1016/j.injury.2012.10.009
Malaktaris, A., McLean, C. L., Mallavarapu, S., Herbert, M. S., Kelsven, S., Bormann, J. E., & Lang, A. J. (2022). Higher frequency of mantram repetition practice is associated with enhanced clinical benefits among United States Veterans with posttraumatic stress disorder. European Journal of Psychotraumatology, 13(1). https://doi.org/10.1080/20008198.2022.2078564
Malarkey, M. E., Fu, A. J., Mannan, N., Shaw, O. M., Haight, T. J., Cota, M. R., … & Brody, D. L. (2024). Internet-Guided Cognitive Behavioral Therapy for Insomnia Among Patients With Traumatic Brain Injury. JAMA Network Open, 7(7), e2420090. https://doi.org/10.1001/jamanetworkopen.2024.20090
Meis, L. A., Noorbaloochi, S., Hagel Campbell, E. M., Erbes, C. R., Polusny, M. A., Velasquez, T. L., … & Spoont, M. R. (2019). Sticking it out in trauma-focused treatment for PTSD: It takes a village. Journal of Consulting and Clinical Psychology, 87(3), 246–256. https://doi.org/10.1037/ccp0000386
Miloradova, N. (2023). Current Assessment Methods of Investigator’s Psychological Readiness for Professional Activities: Improvement Perspectives. Futurity of Social Sciences, 1(2), 45–58. https://doi.org/10.57125/FS.2023.06.20.04
Monson, C. M., Pukay-Martin, N. D., Wagner, A. C., Crenshaw, A. O., Blount, T. H., Schobitz, R. P., … & Peterson, A. L. (2024). Cognitive–behavioral conjoint therapy versus prolonged exposure for PTSD in military service members and veterans: results and lessons from a randomized controlled trial. European Journal of Psychotraumatology, 15(1). https://doi.org/10.1080/20008066.2024.2330305
Paiva, J. M., dos Santos Melani, M., Marques, E. S. N., Arcosy, C. von, Coutinho, E. S. F., Ventura, P., & Berger, W. (2024). The efficacy of internet-delivered cognitive-behavioral therapy for posttraumatic stress disorder according to the mean age of patients: a systematic review and meta-analysis. Psychology, Health & Medicine, 29(4), 683–697. https://doi.org/10.1080/13548506.2023.2292478
Perez Garcia, G., Perez, G. M., Otero-Pagan, A., Abutarboush, R., Kawoos, U., De Gasperi, R., … & Elder, G. A. (2021). Transcranial Laser Therapy Does Not Improve Cognitive and Post-Traumatic Stress Disorder–Related Behavioral Traits in Rats Exposed to Repetitive Low-Level Blast Injury. Neurotrauma Reports, 2(1), 548–563. https://doi.org/10.1089/neur.2021.0005
Peterson, A. L., Foa, E. B., Resick, P. A., Hoyt, T. V., Straud, C. L., Moore, B. A., … & Mintz, J. (2020). A Nonrandomized Trial of Prolonged Exposure and Cognitive Processing Therapy for Combat-Related Posttraumatic Stress Disorder in a Deployed Setting. Behavior Therapy, 51(6), 882–894. https://doi.org/10.1016/j.beth.2020.01.003
Peterson, A. L., Mintz, J., Moring, J. C., Straud, C. L., Young-McCaughan, S., McGeary, C. A., … & Resick, P. A. (2022). In-office, in-home, and telehealth cognitive processing therapy for posttraumatic stress disorder in veterans: a randomized clinical trial. BMC Psychiatry, 22(1), 41. https://doi.org/10.1186/s12888-022-03699-4
Pruiksma, K. E., Cranston, C. C., Rhudy, J. L., Micol, R. L., & Davis, J. L. (2018). Randomized controlled trial to dismantle exposure, relaxation, and rescripting therapy (ERRT) for trauma-related nightmares. Psychological Trauma: Theory, Research, Practice, and Policy, 10(1), 67–75. https://doi.org/10.1037/tra0000238
Pruiksma, K. E., Taylor, D. J., Mintz, J., Nicholson, K. L., Rodgers, M., Young-McCaughan, S., … & Peterson, A. L. (2020). A pilot randomized controlled trial of cognitive behavioral treatment for trauma-related nightmares in active duty military personnel. Journal of Clinical Sleep Medicine, 16(1), 29–40. https://doi.org/10.5664/jcsm.8116
Reijnen, A., Rademaker, A. R., Vermetten, E., & Geuze, E. (2015). Prevalence of Mental Health Symptoms in Dutch Military Personnel Returning from Deployment to Afghanistan: A 2-year Longitudinal Analysis. European Psychiatry, 30(2), 341–346. https://doi.org/10.1016/j.eurpsy.2014.05.003
Resick, P. A., Wachen, J. S., Dondanville, K. A., LoSavio, S. T., Young-McCaughan, S., Yarvis, J. S., … Mintz, J. (2021). Variable-length Cognitive Processing Therapy for posttraumatic stress disorder in active duty military: Outcomes and predictors. Behavior Research and Therapy, 141, 103846. https://doi.org/10.1016/j.brat.2021.103846
Sandweiss, D. A. (2011). Preinjury Psychiatric Status, Injury Severity, and Postdeployment Posttraumatic Stress Disorder. Archives of General Psychiatry, 68(5), 496. https://doi.org/10.1001/archgenpsychiatry.2011.44
Pokharel, S., Pandey, A., & Dahal, S. R. (2024). Globalization, Brain Drain, and its Impact in Nepal. Futurity Philosophy, 3(3), 4–21. https://doi.org/10.57125/FP.2024.09.30.01
Schnurr, P. P., Chard, K. M., Ruzek, J. I., Chow, B. K., Resick, P. A., Foa, E. B., … Shih, M.-C. (2022). Comparison of Prolonged Exposure vs Cognitive Processing Therapy for Treatment of Posttraumatic Stress Disorder Among US Veterans. JAMA Network Open, 5(1), e2136921. https://doi.org/10.1001/jamanetworkopen.2021.36921
Sijbrandij, M., Kunovski, I., & Cuijpers, P. (2016). Effectiveness of internet-delivered cognitive behavioral therapy for posttraumatic stress disorder: a systematic review and meta-analysis. Depression and Anxiety, 33(9), 783–791. https://doi.org/10.1002/da.22533
Skopp, N. A., Kaplan, D. A., Todd, B. L., Drell, M. B., & Pratt, K. M. (2023). Pilot outcomes of cognitive processing therapy implementation in military health system outpatient behavioral health clinics. Psychological Services, 20(3), 496–505. https://doi.org/10.1037/ser0000611
Sloan, D. M., Marx, B. P., Resick, P. A., Young-McCaughan, S., Dondanville, K. A., Mintz, J., … & Peterson, A. L. (2020). Study design comparing written exposure therapy to cognitive processing therapy for PTSD among military service members: A noninferiority trial. Contemporary Clinical Trials Communications, 17, 100507. https://doi.org/10.1016/j.conctc.2019.100507
Sloan, D. M., Marx, B. P., Resick, P. A., Young-McCaughan, S., Dondanville, K. A., Straud, C. L., … & Peterson, A. L. (2022). Effect of Written Exposure Therapy vs Cognitive Processing Therapy on Increasing Treatment Efficiency Among Military Service Members With Posttraumatic Stress Disorder. JAMA Network Open, 5(1), e2140911. https://doi.org/10.1001/jamanetworkopen.2021.40911
Song, J., Johnson, C., Suvak, M. K., Shields, N., Lane, J. E. M., Monson, C. M., & Wiltsey-Stirman, S. (2020). Patterns of change in physical functioning and posttraumatic stress disorder with cognitive processing therapy in a randomized controlled implementation trial. European Journal of Psychotraumatology, 11(1), 1801166. https://doi.org/10.1080/20008198.2020.1801166
Steenkamp, M. M., Litz, B. T., Hoge, C. W., & Marmar, C. R. (2015). Psychotherapy for Military-Related PTSD. JAMA, 314(5), 489. https://doi.org/10.1001/jama.2015.8370
Sundin, J., Herrell, R. K., Hoge, C. W., Fear, N. T., Adler, A. B., Greenberg, N., … & Bliese, P. D. (2014). Mental health outcomes in US and UK military personnel returning from Iraq. British Journal of Psychiatry, 204(3), 200–207. https://doi.org/10.1192/bjp.bp.113.129569
Tanev, K. S., Federico, L. E., Greenberg, M. S., Orr, S. P., Goetter, E. M., Resick, P. A., & Pitman, R. K. (2020). Baseline Cognitive Performance and Treatment Outcomes From Cognitive-Behavioral Therapies for Posttraumatic Stress Disorder: A Naturalistic Study. The Journal of Neuropsychiatry and Clinical Neurosciences, 32(3), 286–293. https://doi.org/10.1176/appi.neuropsych.19020032
Taylor, D. J., Peterson, A. L., Pruiksma, K. E., Young-McCaughan, S., Nicholson, K., & Mintz, J. (2017). Internet and In-Person Cognitive Behavioral Therapy for Insomnia in Military Personnel: A Randomized Clinical Trial. Sleep, 40(6). https://doi.org/10.1093/sleep/zsx075
Windle, E., Tee, H., Sabitova, A., Jovanovic, N., Priebe, S., & Carr, C. (2020). Association of Patient Treatment Preference With Dropout and Clinical Outcomes in Adult Psychosocial Mental Health Interventions. JAMA Psychiatry, 77(3), 294. https://doi.org/10.1001/jamapsychiatry.2019.3750
Zaitsev, S. (2023). The role of management accounting in the sustainable development of small enterprises: an analytical review of challenges and opportunities. Law, Business and Sustainability Herald, 3(1), 33–45. Retrieved from https://lbsherald.org/index.php/journal/article/view/42
https://amazoniainvestiga.info/ ISSN 2322- 6307

This article presents no conflicts of interest. This article is licensed under the Creative Commons Attribution 4.0 International License (CC BY 4.0). Reproduction, distribution, and public communication of the work, as well as the creation of derivative works, are permitted provided that the original source is cited.